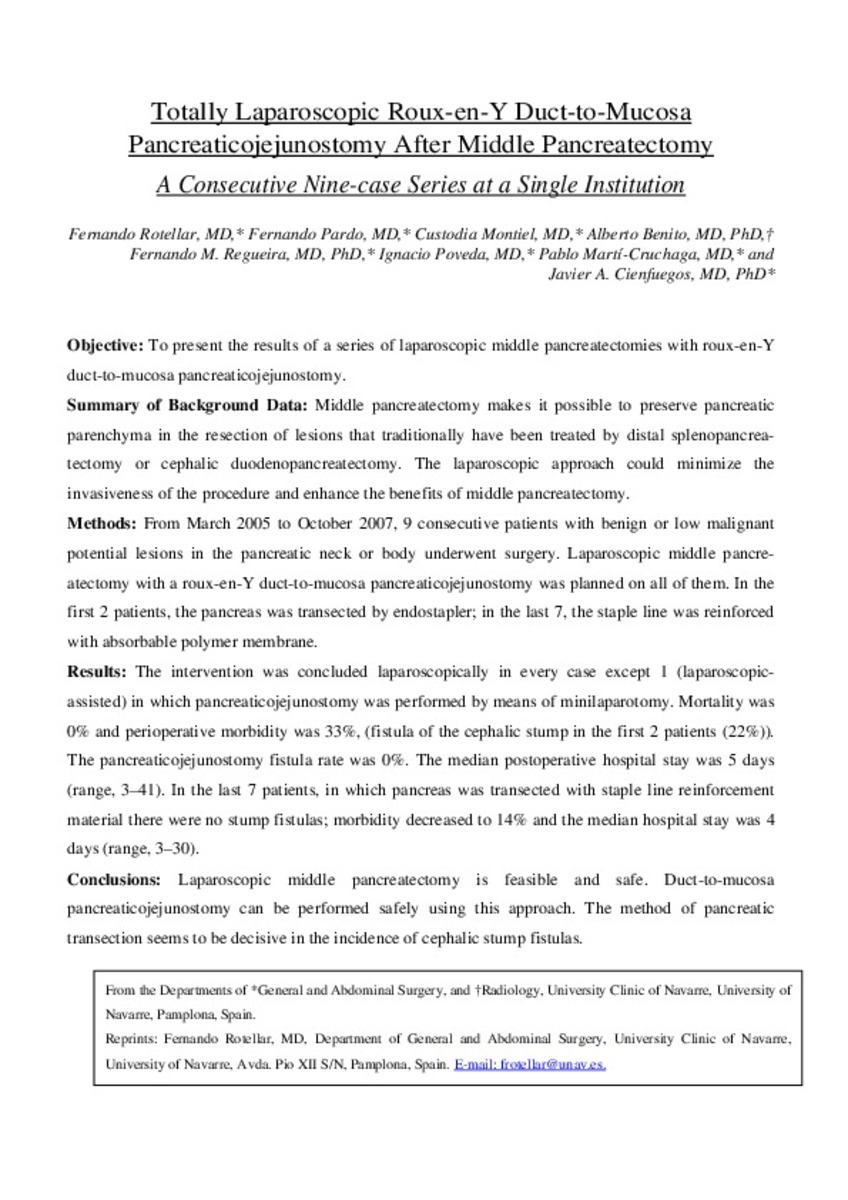
Totally Laparoscopic Roux-en-Y Duct-to-Mucosa Pancreaticojejunostomy After Middle Pancreatectomy A Consecutive Nine-case Series at a Single Institution
Keywords:
Anastomosis, Roux-en-Y
Pancreatectomy/methods
Pancreatic Neoplasms/diagnosis/surgery
Publisher:
Lippincott, Williams & Wilkins
Citation:
Rotellar F, Pardo F, Montiel C, Benito A, Regueira FM, Poveda I, et al. Totally laparoscopic Roux-en-Y duct-to-mucosa pancreaticojejunostomy after middle pancreatectomy: a consecutive nine-case series at a single institution. Ann Surg 2008 Jun;247(6):938-944.
Statistics and impact
0 citas en

0 citas en

Items in Dadun are protected by copyright, with all rights reserved, unless otherwise indicated.