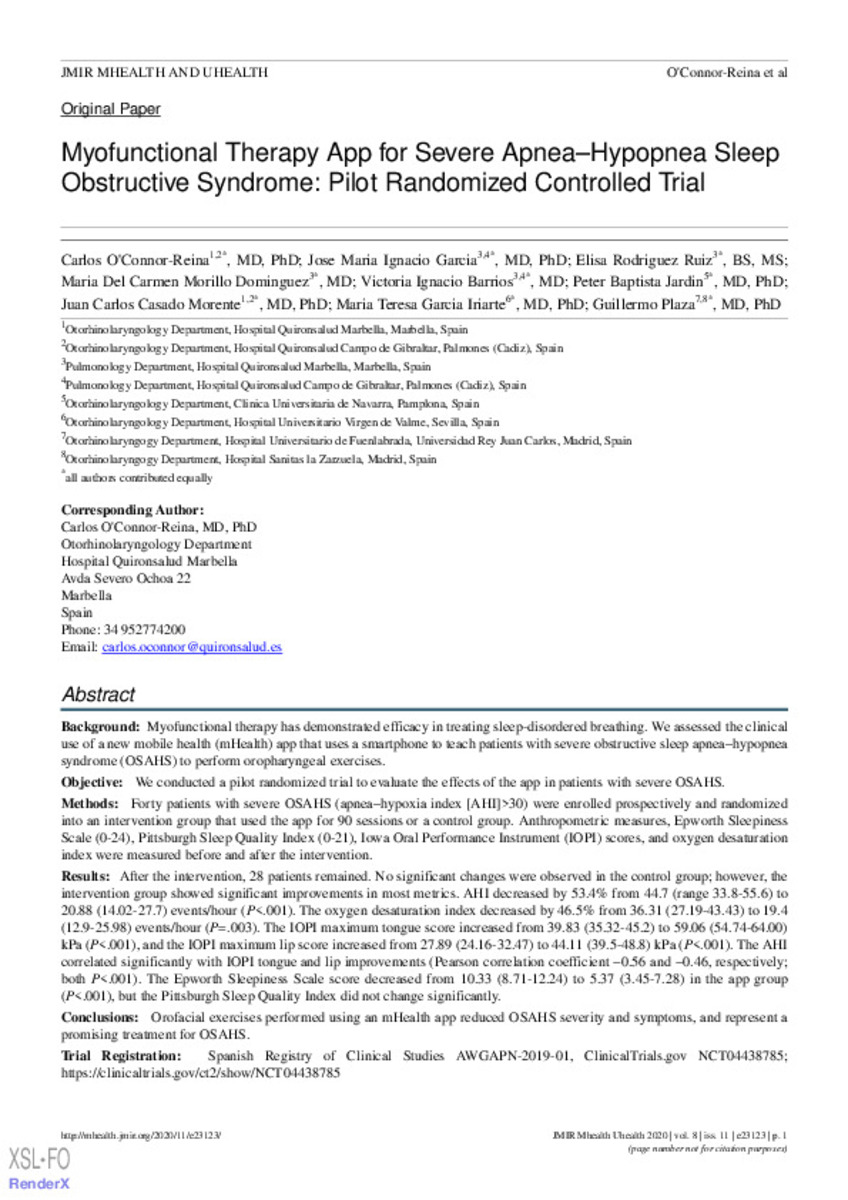
Myofunctional therapy app for severe apnea-hypopnea sleep obstructive syndrome: Pilot randomized controlled trial
Keywords:
Myofunctional therapy
Oropharyngeal exercises
mHealth
Sleep apnea
Smartphone app
App
Sleep
Therapy
Apnea
Randomized trial
Efficacy
Note:
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR mHealth and uHealth, is properly cited. The complete bibliographic information, a link to the original publication on http://mhealth.jmir.org/, as well as this copyright and license information must be included.
Citation:
O’Connor-Reina, C. (Carlos); Garcia, J.M.I. (José Maria Ignacio); Rodriguez-Ruiz, E. (Elisa); et al. "Myofunctional therapy app for severe apnea-hypopnea sleep obstructive syndrome: Pilot randomized controlled trial". JMIR mHealth and uHealth. 8 (11), 2020, e23123
Statistics and impact
0 citas en

0 citas en

Items in Dadun are protected by copyright, with all rights reserved, unless otherwise indicated.