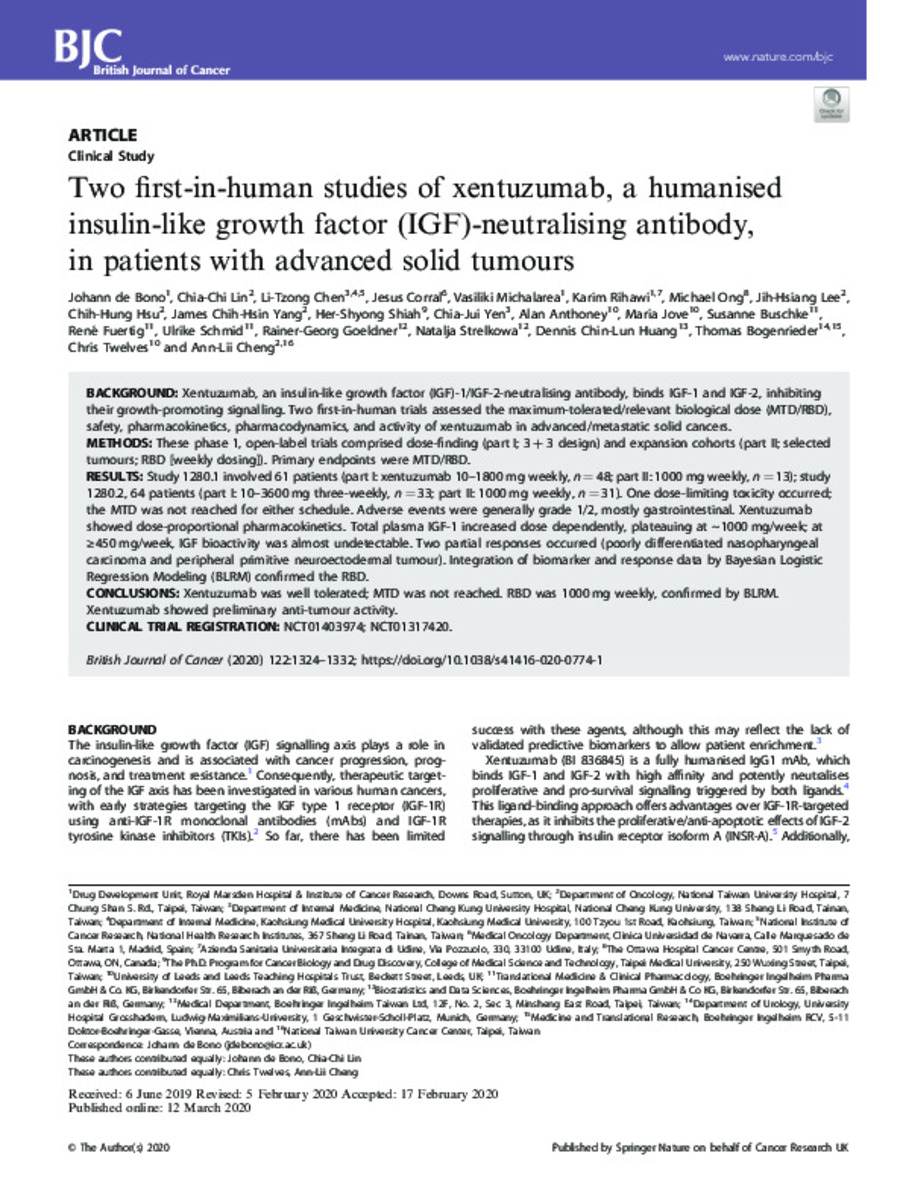
Two first-in-human studies of xentuzumab, a humanised insulin-like growth factor (IGF)-neutralising antibody, in patients with advanced solid tumours
Keywords:
Xentuzumab
Insulin
Biological dose
Publisher:
Springer Nature
Note:
This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits use, sharing,
adaptation, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative
Commons license, and indicate if changes were made. The images or other third party
material in this article are included in the article’s Creative Commons license, unless
indicated otherwise in a credit line to the material. If material is not included in the
article’s Creative Commons license and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly
from the copyright holder. To view a copy of this license, visit http://creativecommons.
org/licenses/by/4.0/.
Citation:
Bono, J. (Johann) de; Lin, C.C. (Chia-Chi); Chen, L.T. (Li-Tzung); et al. "Two first-in-human studies of xentuzumab, a humanised insulin-like growth factor (IGF)-neutralising antibody, in patients with advanced solid tumours". British journal of cancer. 122 (9), 2020, 1324 - 1332
Statistics and impact
0 citas en

0 citas en

Items in Dadun are protected by copyright, with all rights reserved, unless otherwise indicated.